Breast Procedures


Overview of Breast Reconstruction
(scroll to the bottom for photos)
The loss of a breast to breast cancer is one of the most difficult challenges a woman can face, and it is a fairly common challenge - in the United States, one in eight women will develop breast cancer over her lifetime. There is good news, however - a woman's chance of living a long life after breast cancer has increased dramatically over the past sixty years. Plastic surgeons have also made great progress in rebuilding breasts lost to mastectomy, and unless your health is very poor, most women are candidates for some type of reconstruction.
Removal of the breast can be a serious blow to a woman's self-image and femininity. We hear many common questions: how will my clothes fit? Will I be able to wear a swimsuit? What about intimacy with my spouse or significant other? We can help you address all these concerns, and for most patients we have very encouraging answers.
Dr. Haynes has two areas of particular interest - breast surgery, and facial rejuvenation. He recently published a new technique in breast reconstruction, and has several on-going projects regarding new breast reconstruction techniques. (And you're welcome to ask about these during your visit.)
Breast Reconstruction Techniques
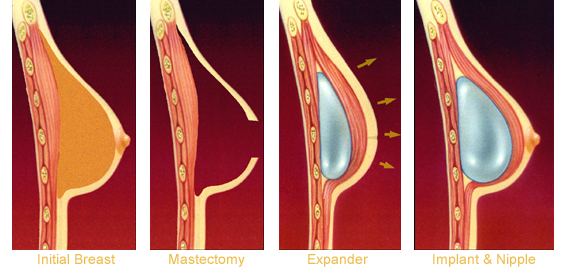
Tissue Expansion: There are several ways of rebuilding a breast, but the most common technique used today is tissue expansion. Following the mastectomy, the plastic surgeon inserts a temporary breast implant, called a tissue expander, beneath the skin and muscle of the chest. Initially, this expander is mostly deflated, to allow the skin to heal after surgery. Then, every week or two, salt water is injected into the expander, slowly stretching the skin and tissue and creating space for a real breast implant. One advantage of using a tissue expander is that the patient gets to choose her breast size.
Once the expander is fully inflated, it is removed (in an outpatient surgery), and a saline or silicone breast implant is inserted. The nipple and areola are also rebuilt, and a simple tattoo procedure in our office provides color.
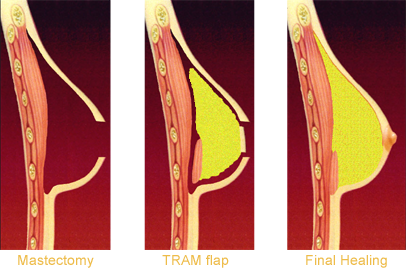
Flap Reconstruction: In this method, a portion of skin and muscle from someplace else on the body is transferred to the breast, and used to replace part or all of the missing tissue after the mastectomy. (Most of the skin on our bodies gets its blood supply from the muscles that are underneath - taking part of a muscle, with the skin over it, is called a flap.)
The flap may come from either the back (using part of the latissimus muscle) or the abdomen (called a TRAM flap). In some cases, a small implant is used under the flap to give more volume or produce a better shape.
Delayed vs. Immediate: The process of breast reconstruction can begin at the same time as the mastectomy - this is called an "immediate" breast reconstruction. There are benefits to starting the reconstruction at the same time, including one less surgery, and the ability to save more of the existing skin on the breast. If a woman has already had mastectomy in the past, that is a "delayed" reconstruction. Many of the techniques used are the same, although it may take more time to stretch the skin than for an immediate reconstruction.
What can you expect from surgery?
As with any surgery, there is some initial pain and discomfort. You can expect to be sore for several weeks afterwards - this is quite normal. A surgical drain is often used to remove accumulated fluid and blood, and is removed after the first week or two. We encourage you to be up walking right away, and within a few days most patients feel well enough to go out to eat, or do light errands. Patients generally are able to return to work in about two weeks, unless the job is physically strenuous.
How long will it take to be all done?
The time course of breast reconstruction depends on many things - for instance, if a woman needs chemotherapy or radiation, that will add some extra time. In most cases though, the entire procedure from start to finish can be done in eight to nine months. We like to tell patients that reconstruction is a process, not an event - but at each step the new breast looks better. Our ultimate goal is this: you can go to the beach, put on a swimsuit, and no one will ever know you had a mastectomy.
Will insurance cover my breast reconstruction?
Yes - insurance is required to cover breast reconstruction after mastectomy, due to a federal law called the Women's Health and Cancer Rights Act of 1998.
Has Dr. Haynes done many breast reconstructions?
Dr. Haynes has done close to 1000 breast reconstructions in his career - and as mentioned above, it is his primary research interest, and he has helped contribute to the latest techniques.
What are the risks of surgery?
Breast reconstruction has the same basic risks as other types of surgery - you could have bleeding, develop an infection, be nauseated afterwards, or become allergic to a drug. Specific risks about breast reconstruction are: 1) if an implant becomes infected, it usually needs to be temporarily removed; 2) scar tissue can form around an implant, making it feel firm, or altering its shape; and 3) breast implants are not guaranteed to last forever, and may need to be replaced at some point in the future.
What if I smoke?
If you smoke, it is often best to delay the reconstruction until after the mastectomy is well healed, and you have completed any necessary "adjuvant" treatment, such as radiation or chemotherapy. The nicotine in cigarettes can interfere with blood supply to the skin, increasing the risk of poor healing or tissue loss. It is much preferred to quit smoking before reconstruction is done.
Do my breasts have to be the same size as they are now? Can I go larger or smaller?
In most cases yes - you can go either larger, or smaller, whichever you prefer. As you can see from the photos below, going larger is a popular choice.
Will reconstruction change the risk of the breast cancer coming back?
Long-term studies have shown that breast reconstruction has no effect on recurrence of breast cancer - it is not more likely to come back, or less likely to come back. But reconstruction does make having had a mastectomy a lot easier to live with.
Should I have both breasts removed, or just the one?
This is a complicated question, and one that we try to individualize for each patient. No woman wants to lose a breast unnecessarily. If your risk of getting breast cancer in the other breast is very low, you may want to keep it - it is, after all, yours, and has been part of you since puberty. Many women do choose, however to have both breasts removed - there is less worry of developing a problem in the other breast, and when doing reconstruction, we can make the two breasts match better if we rebuild both of them the same way.
What is my next step?
Dr. Haynes is happy to talk with you at any point in the process of treatment. If you have just had a biopsy, and been told you have cancer, you are welcome to call us right away. We can help you select a general surgeon, and start planning the process of care. If you had mastectomy years ago, and are just curious about your options - again, give us a call, and we are happy to visit with you. We have many, many patients who have been through breast cancer treatment and reconstruction, and who are willing to share their experience with you - if you'd like to talk to someone who's been through it, give us a call and we'll set it up for you.

Breast Reconstruction Photos - before & after
move pointer over photos to enlarge
41 year old patient, bilateral skin-sparing mastectomy. Reconstruction with bilateral latissimus flaps and expanders, then silicone implants and nipple reconstruction.
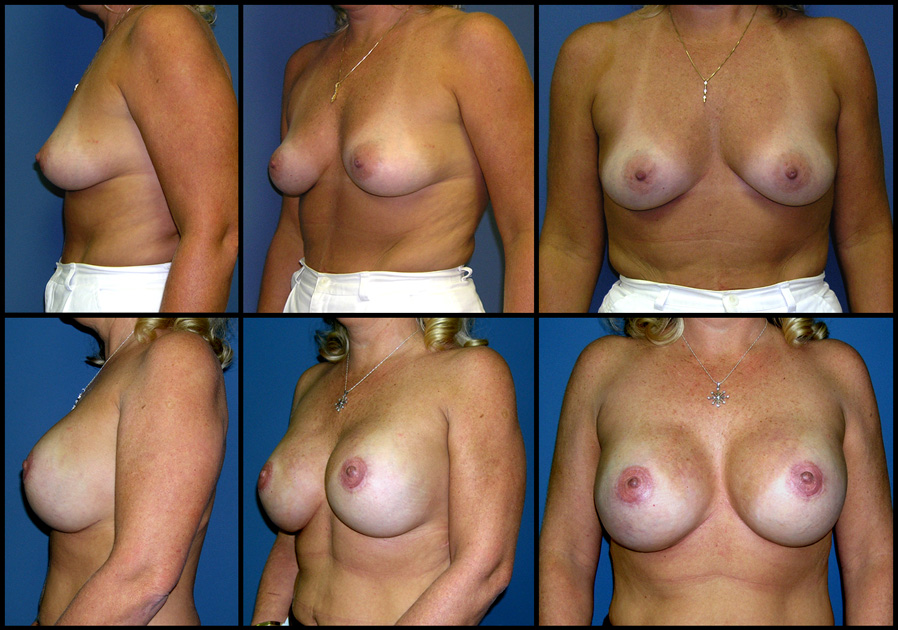
Postop photos taken 4 months after final surgery
34 year old patient, bilateral areola-sparing mastectomy (by Dr. Beth Lawson). Reconstruction with tissue expanders, then silicone implants.
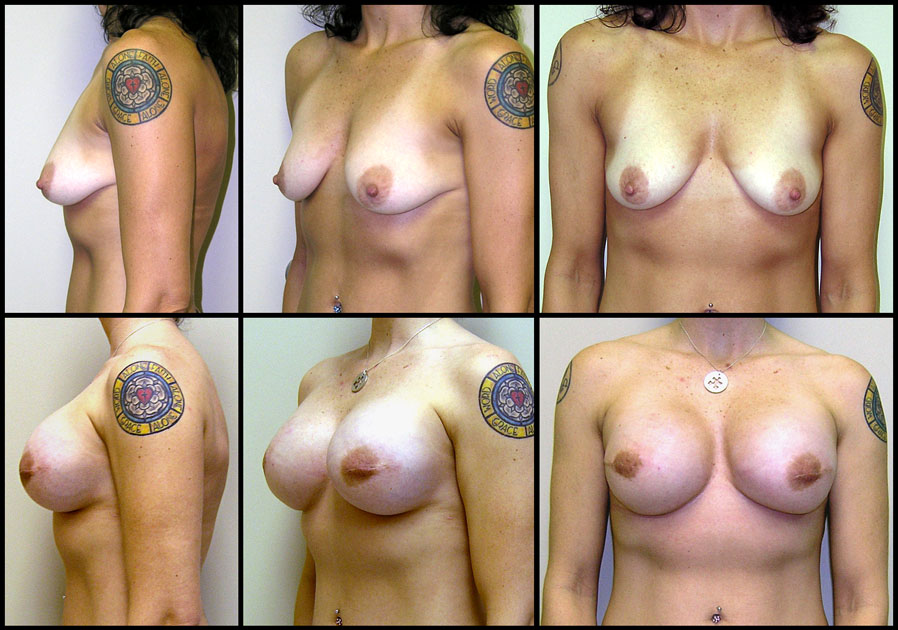
Postop photos taken 1 month after final surgery
35 year old patient, bilateral skin-sparing mastectomy. Reconstruction with bilateral tissue expanders and Vicryl mesh, then silicone implants and nipple reconstruction.
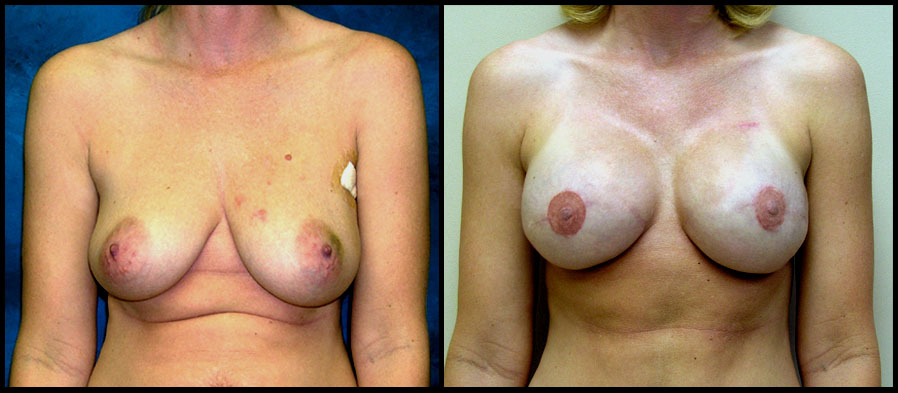
Postop photo taken 10 months after final surgery
49 year old patient after bilateral mastectomy. Delayed reconstruction with bilateral tissue expanders, then silicone implants and nipple reconstruction.
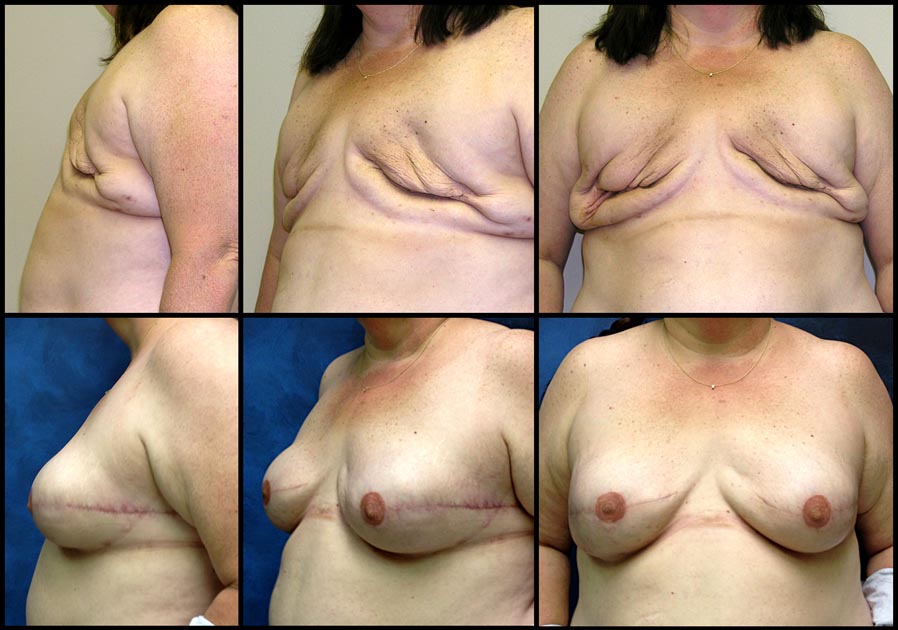
Postop photo taken 2 months after final surgery
An important disclaimer:
We show representative photos, which are for information purposes only. The pictures do not constitute any guarantee or promise of specific results.
We'll do our best to make you look good, but we can't make you look exactly like one of the photos.
We use no stock photography. All photographs on this website are of actual patients.